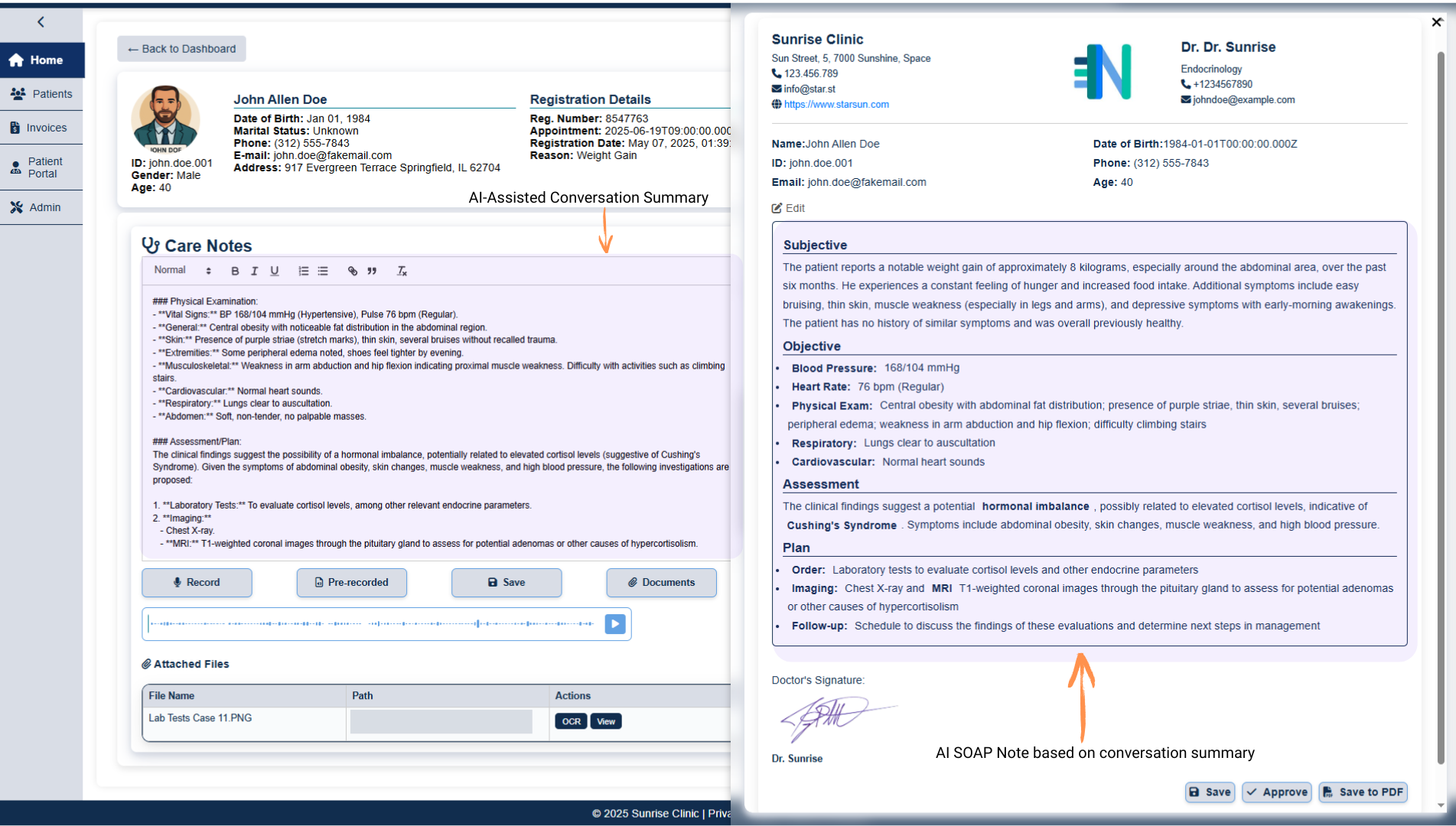
From mic to medical record: AI-generated SOAP notes in seconds
Still spending 15 minutes typing SOAP notes? Watch Nexpert’s AI craft the entire Subjective-Objective-Assessment-Plan in one click—ready to save or export.

Picture this scenario
A clinician’s exam room is often the quiet eye of a storm. Outside, phones ring, beds fill, and inboxes overflow. Inside, the practitioner strives to listen, diagnose, reassure—and then faces the second shift: translating the encounter into a structured SOAP note.
Subjective, Objective, Assessment, Plan… the acronym is simple, the work is not. Studies peg the average post-visit documentation time at 11-16 minutes per patient, devouring evenings and weekends.


Nexpert Solutions thinks those hours belong back with providers and patients. Its new AI-Assisted SOAP Note module turns a raw audio recording into a polished, four-part note with a single click.
The process is so fast it feels like sorcery; in reality, it is the convergence of speech recognition, large-language models, and template-level precision.


From conversation to transcript
The workflow starts exactly where care happens: the dialogue between clinician and patient. Whether you record directly in Nexpert’s mobile app or upload audio afterward, state-of-the-art speech-to-text renders a word-perfect transcript in seconds. Accents, rapid exchanges, even overlapping speech are handled automatically.


One button, four sections
SOAP Note
With the transcript ready, the user hits Generate SOAP Note. In the time it takes to sip coffee, Nexpert’s GPT-4o assistant parses the conversation and slots each detail into the canonical structure:
- Subjective – the patient’s own words: “I’ve had stabbing pain in my left knee for three weeks.”
- Objective – vitals, exam findings, any point-of-care tests.
- Assessment – the clinician’s impression: e.g., “likely meniscal tear.”
- Plan – imaging orders, medication changes, follow-up timeline.
The draft appears with inline editing enabled. Providers tweak phrasing, add a code, or reorder bullet points, then click Save—immediately attaching the note to the electronic health record (EHR) or exporting a PDF for external teams.

Why it matters
- Clinician well-being: Reducing after-hours charting is the single biggest predictor of burnout improvement, according to AMA surveys.
- Revenue integrity: Structured notes feed directly into coding; fewer missed modifiers means cleaner claims and faster payment cycles.
- Clinical quality: Consistent SOAP formatting helps downstream readers—nurses, PTs, specialists—find critical information instantly.


Behind the curtain: How the AI “thinks”
1. Entity extraction pulls problems, medications, dosages, and exam findings from free text.
2. Template mapping aligns each entity to the correct SOAP heading.
3. Clinical heuristics ensure the note reflects medical logic—e.g., a medication listed in Plan must appear in Assessment or Objective first.
4. Quality guardrails flag contradictions (“no fever” vs. 38.9 °C) for the provider to review.
Because the model never invents data, every line traces back to the original transcript. That audit trail satisfies both internal QA and external regulators.

Integration without upheaval
Nexpert’s SOAP module installs as a plug-in inside the existing platform. For organizations on Epic, Cerner, or other major EHRs, a FHIR-based connector writes notes back automatically—no copy-paste required. Permissions mirror the host system, so trainees can draft while attendings approve. Deployment typically follows a three-step path:
1. Pilot: one service line (e.g., orthopedics) for two weeks.
2. Scale: roll out to all ambulatory clinics.
3. Optimize: enable auto-coding and analytics dashboards.


Beyond SOAP: A gateway to fully AI-enabled documentation
The same engine driving SOAP generation already powers Nexpert’s appointment transcripts and medical coding modules.
Turning it on today lays the foundation for tomorrow’s auto-generated discharge summaries, referral letters, even patient education leaflets—each built from the same source of truth: the recorded encounter.


Ready for a closer look?
The two-minute video demo brings the workflow to life—watch a transcript morph into a complete note before your eyes. Then picture your own team trading late-night typing for genuine downtime or extra patient slots.
Want to see it live? Reach out and the Nexpert team will arrange a sandbox session tailored to your specialty. Because the future of clinical documentation isn’t more typing—it’s less.

How the Latest AI Tools Can Help the Modern Healthcare Landscape
Let's talk
If you lead IT, operations, or revenue cycle in BENELUX or DACH, schedule a 20-minute discovery call and see a live demo on your own dataset.
